Immediate changes to the Network Contract DES
Following on from lessons learned through last winter and the pandemic to support practice capacity and PCN development, the following changes are being made.
Issuing a variation to the Network Contract DES to make several changes:
- introducing flexibility into the Additional Roles Reimbursement Scheme (ARRS) including the addition of a GP assistant role and a digital and transformation lead role
- retiring or deferring to 2023/24 four investment and impact fund (IIF) indicators and allocating this funding to PCNs via a monthly PCN capacity and access support payment, for the purchase of additional clinical services or workforce
- reducing the thresholds of two IIF indicators and changing the definition of a further two IIF indicators
- removing the personalised care requirement for all clinical staff to undertake the Personalised Care Institute’s e-learning refresher training for shared decision making (SDM) conversations
- making changes to the anticipatory care requirements to reflect the revised national approach of phased implementation of this model of care from April 2023.
NHS England is committed to supporting the long-term development of neighbourhood multi-disciplinary teams in primary care. Staff recruited via the ARRS are central to this ambition.
In 2020, NHS England advised that ARRS-recruited staff will be treated as part of the core general practice cost base beyond 2023/24.
Permanent contracts (where appropriate) could be offered by PCN employers.
PCNs are encouraged to continue to recruit, making full use of their ARRS entitlement with the knowledge that support for these staff will continue.
Further support for general practice and PCNs during winter 22/23
Updates to the ARRS
1. Introduce a general practice assistant (GPA) role in the ARRS. The role will offer clinical and administrative support to GPs, freeing up clinical time to focus on patient care. The role will be subject to a maximum reimbursement equivalent of an Agenda for Change Band 4 level and the outline will be based on the HEE competency framework.
PCNs can immediately start recruiting to the role, predominantly through trainee positions. Staff can be trained in-practice, with on-the-job training and development led by GPs, in line with the role outline. Trainee GPAs will also have the opportunity to complete HEE’s structured, accredited training route, aligned to the competency framework, equipping them with formal certification of their learning.
2. Introduce a digital and transformation lead, to support increased access to care for patients, by supporting the adoption and/or optimisation of new technology and other initiatives to improve the care offer, and enabling PCN staff to work more effectively to support the sustainability of general practice services. The role will be capped at one per PCN and maximum reimbursement will be equivalent to an Agenda for Change band 8a. It will include delivery of a combination of the following responsibilities:
- Improve adoption and/or optimisation of new technology to enhance patient access and experience and increase PCN productivity
- Build relationships and facilitate collaboration between practices and the wider system to support the delivery of care to patients (including shared appointments between practices to aid delivery of enhanced access)
- Lead an improvement approach to change including building capability for quality improvement within the PCN and system wide approaches to problem solving
- Review and improve the PCN’s digital maturity
- Use data, and improve data quality, to:
- i. understand demand, capacity and activity and drive improvements in:
- patient experience of access
- operational efficiency including better matching capacity to need
- staff experience at work.
- ii. support population health management
- iii. support understanding of the type and intensity of support/training needs of the PCN and coordinate this support, including through OD programmes
- iv. facilitate clinically led innovation and the effective adoption of improvement initiatives, including integrated working at neighbourhood and/or place level to improve access to services for patients.
- i. understand demand, capacity and activity and drive improvements in:
- Use data, and improve data quality, to:
3. Increase the current cap on hiring advanced practitioners (APs) through the ARRS, from one per PCN to two (double for those with over 100,000 patients). APs are able to supervise members of the multidisciplinary team (MDT) and see undifferentiated patients, supporting workload reduction from GPs.
4. Reimburse training time for nursing associates to become registered nurses who work in general practice, enabling PCNs to develop their nursing workforce and providing a career path for nursing associates. For April 2023 onwards, we will also consider support for senior nurses within PCNs.
5. Increase the ARRS maximum reimbursement rates for 2022/23 to account for the Agenda for Change uplift.
6. Remove the minimum 0.5 FTE restriction on clinical pharmacists once they have completed their required 18-month training course or have
been granted equivalence/exemption from the PCPEP pathway.
7. Contractually permit equivalent entry routes to PCPEP for pharmacy technician role. This will formalise the exemptions that PCPEP apply to some pharmacy technicians who already have the requisite skills.
Updates to the PCN service specifications
8. Update the anticipatory care requirements to better reflect system-level work on anticipatory care. Replace the current specification with:
- 8.9.1. ICSs have responsibility to design and plan anticipatory care for their system, of which the following PCN requirements form a part.
- 8.9.2. PCNs must contribute to ICS-led conversations on the local development and implementation of anticipatory care working with other providers with whom anticipatory care will be delivered jointly.
9. Remove the personalised care requirement for all clinical staff to undertake the Personalised Care Institute’s 30-min e-learning refresher training for SDM conversations.
Updates to IIF incentives
10. Defer the following indicators to 2023/24:
- ACC-02: Number of online consultation submissions received by the PCN per registered patient.
- EHCH-06: Standardised number of emergency admissions on or after 1 October per care home resident aged >= 18.
- IIF ACC-08: Percentage of patients whose time from booking to appointment was two weeks or less.
11. Retire IIF ACC-05: By 31 March 2023, make use of GP Patient Survey results for practices in the PCN to (i) identify patient groups experiencing inequalities in their experience of access to general practice, and (ii) develop, publish and implement a plan to improve patient experience and access for these patient groups, taking into account demographic information including levels of deprivation.
12. In total, the above equals £37m of funding to be released to PCNs as a PCN Support Payment. The PCN Support Payment will be paid on a monthly basis and will be based on the PCN’s Adjusted Population. In line with the reinvestment commitment relating to IIF earnings, the PCN capacity and access support payment must be used to purchase additional workforce and increase clinical capacity to support additional appointments and access for patients.
13. Amend the thresholds of the following indicators to better reflect operational realities:
- IIF CVD-02: Increase in percentage of registered patients on the QOF Hypertension Register: This indicator is closely linked to IIF CVD-01 which recognises PCNs for following up elevated blood pressure readings to confirm or exclude hypertension. Reduce the 22/23 thresholds to from 0.6/1.2 to 0.4/0.8 percentage point increase.
- IIF PC-01: Percentage of registered patients referred to a social prescribing service. Reduce 22/23 thresholds from 1.2%/1.6% to 0.8%/1.2%.
14. Amend the wording of the following IIF indicators based on feedback from the first half of the year to make them easier to achieve:
- CAN-01, which recognises PCNs for ensuring that lower gastrointestinal fast-track referrals for suspected cancer are accompanied by a faecal immunochemical test or FIT – change permissible time between FIT result and referral from seven to twenty-one days.
- CVD-04, which recognises PCNs for referring patients with high cholesterol for assessment for familial hypercholesterolaemia – expand list of success criteria to include diagnoses of secondary hypercholesterolaemia, genetic diagnoses of familial hypercholesterolaemia, and assessments for familial hypercholesterolaemia, in addition to referral for assessment for familial hypercholesterolaemia.
Financial incentives for autumn vaccination of care homes
A financial incentive is available up until 23rd October 2022 to general practice and community pharmacy providers to prioritise the COVID-19 vaccination of care home residents. To claim the incentive payment providers will need to complete a survey, within 48 hours of the visit, setting out how many residents have been vaccinated and how many have declined, or where a personalised care adjustment applies (for example, where there is a clinical reason that a patient cannot be vaccinated).
GP Postgraduate Doctors in Training (GP Trainees)
Applying to join the Medical Performers List at the right time (and not before).
As you may be aware, you are required to be included in the English Medical Performers List to work independently in NHS general medical practice in England. The regulations have been amended during the Covid-19 pandemic, such that GP Trainees are NOT required to be on the Performers list, and only need to take action to join at the end of their training programme as outlined below.
Please apply at the right time, as applying too early will not lead to your joining the list, and will cause additional unnecessary administration for you and the supporting teams with whom we closely work.
It is anticipated that upcoming changes to the Regulations will make this permanent, hence you should follow this advice until further notice:
- For STI and ST2 trainees:
- Please do not apply to the Performers List at this stage. Due to the Covid-19 amendment to the Performers List Regulations, GPRs are not required to be on the Performers List whilst in training. Whilst this is a temporary amendment, it is anticipated that upcoming changes to the Regulations will make this permanent.
- For ST3 trainees:
- Your name may already be included on the List as arrangements may previously have been made for your inclusion on the List either before you started training or whilst you were in training, prior to the Pandemic rules. You can check if your name is already on the Performers List here Search – Performers List for England.
- If your name is not already included on the Performers List you will need to make an application to join it, but NOT BEFORE you are within 6 calendar months of your anticipated CCT date.
- ST3 trainees only should submit an application to join the Performers List no later than 3 months prior to CCT.
- In other words, you should only complete your application between 6 and 3 months BEFORE your expected CCT date. If the application is started too late, it may result in you not being able to work immediately as an independent qualified GP.
- You can start your PCSE Online application form here PCSS: Login (england.nhs.uk) An application user guide, including information on how to register for an account and a list of documentation you need to upload as part of the application process, can be found here – performer list application guide.
- For all newly qualified GPs:
- Once you have your CCT, please log into PCSE Online and change your status to GP Performer. Further details of now to do this can be found here: General enquiries – Primary Care Support England
MuM-PreDiCT study
Dr Steph Hanley and is a Research Fellow at the University of Birmingham working on the MuM-PreDiCT project. She is interested in speaking with women who are pregnant or postpartum and are living with multimorbidity, their partners, and staff who provide their care. To date, whilst there are many examples of research exploring individuals’ experiences and care pathways for pregnancy with a single morbidity, there is very little research exploring the experiences and care of women managing multiple health conditions. So, as part of this project, they aim address this gap, so that care and pathways can be improved to better meet the needs of women, their babies, and families.
They have been conducting interviews for around 6 months, and are now especially interested in speaking with GPs. It is very important that they understand the views of a range of healthcare professionals who provide antenatal and postnatal care to women with multimorbidity, and recommendations for improvements to future NHS care provision can be made that reflect the experiences and barriers of all relevant staff.
Taking part would involve GPs participating in a short online/in-person interview, depending on their preference. More information about the project can be found here: https://mumpredict.org/.
Contact Dr Hanley via mumpredict@contacts.bham.ac.uk
Advice for managing long COVID with GP staff
While the symptoms may vary, and the diagnosis may be slow to be confirmed, long COVID is most likely to be categorised as a disability in employment terms. This means that, as an employer, you must take extra care in managing the employment relationship – not just managing the absences themselves but also in the day-to-day management of staff affected, to ensure employees are not suffering a detriment as a result of their condition. Investing time and skill early in the process can reduce the long-term liabilities of the practice and encourage a supportive working environment. Talk to the BMA’s Employment Advisory Service to get support with your staff employment issue Employer Advisory Service (bma.org.uk)
Three ways the BMA can support GPs managing HR issues
As a GP partner or practice manager, your BMA membership includes HR and employment law advice and practical support.
Read Three ways the BMA can support GPs managing HR issues | BMA blogs to find out how they can help with:
- non-compliant contracts
- resolving relationship grievances
- untangling complex procedures.
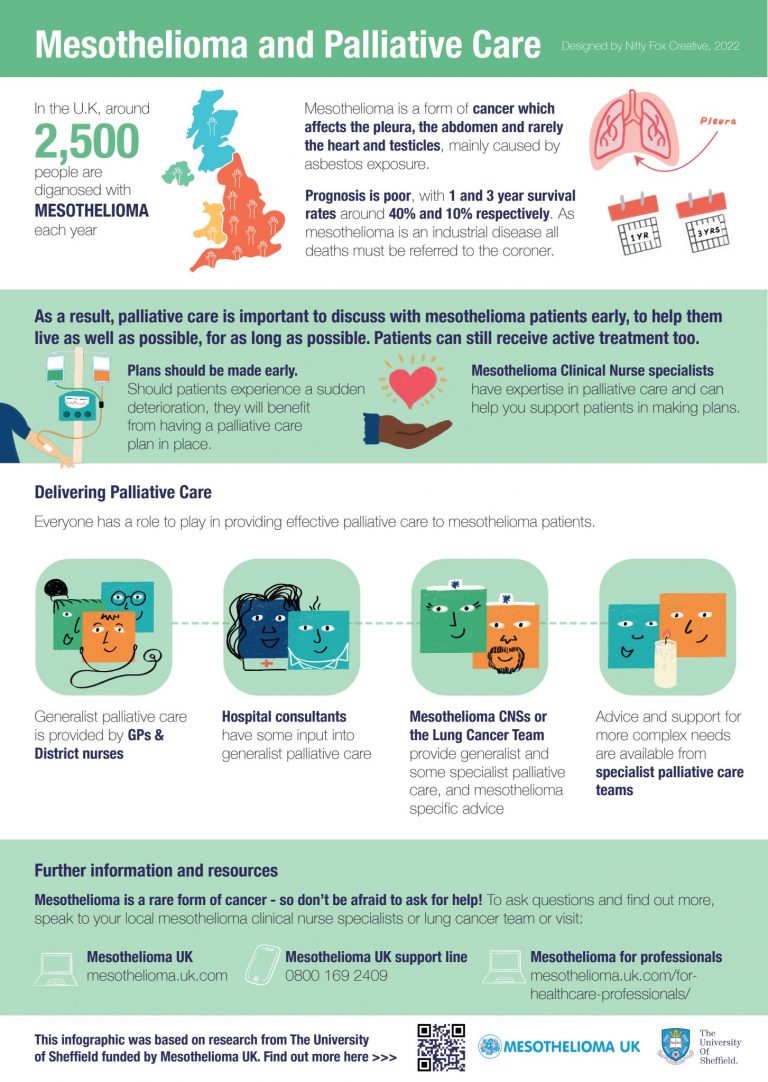
Palliative care for people living with mesothelioma and their families: animation & infographic
The Mesothelioma UK Research Centre have been doing some work to improve palliative care for people living with mesothelioma and their families.
They have launched new tools to help both patients and their families, and healthcare professionals providing care and support.
The tools have been developed out of research findings, a collaboration with the charity Mesothelioma UK, Donna Wakefield (Consultant in Palliative Medicine), and Patient and Public Involvement Group.
The aim is to improve uptake of early-stage palliative care for patients and families, and to empower healthcare professionals in the provision of timely and coordinated care.
The tools are: –
1. Palliative care animation
The short animation aims to demystify palliative care, address common misconceptions, and explain in a sensitive way what palliative care is and how it can help.
Healthcare professional link: https://www.mesothelioma.uk.com/for-healthcare-professionals/palliative-care/ or https://vimeo.com/732287339
Patient/family link: https://www.mesothelioma.uk.com/palliative-care/
Please feel free to use the animation in any way you wish, such as: putting the animation on your website, signposting people to view it, or using the animation to open conversations about palliative care.
2. Palliative care infographic
The infographic aims to provide information and support for healthcare professionals providing care for patients with mesothelioma and their families.
Mesothelioma is a rare condition, and thus it is important that healthcare professionals are supported in providing palliative care for this patient group, so that care can be timely and well-coordinated.
Please feel free to share this infographic in any way you wish, such as: putting it on your website, or using it as a discussion tool for staff training.
Sheffield University would be very interested to find out the impact of the animation / infographic on patients’ and families’ lives so that they can document the impact of the research. Please email them, if you capture any stories of positive or negative impacts.
Further information
Information about the Palliative Care study can be found on their website: https://www.sheffield.ac.uk/murc/our-research/palliative-care-and-role-clinical-nurse-specialist
If you have any comments, or wish to discuss the research, please get in touch with: –
Angela Milton
Research Project Administrator
Health Sciences School
Division of Nursing and Midwifery
The University of Sheffield – Telephone 0114 222 2211
Change in contribution Rates and introduction of the 10 week rule
The Department of Health and Social Care (DHSC) has announced it is introducing changes to the amount members pay towards their NHS pension. See here for details.
PCSE Online will undergo a system change on 27 October 2022 to implement the new contribution rates. This will be followed by a dedicated technical process to automatically apply the new contribution rates to members’ records to avoid practices having to submit a new Estimate form.
Adjustments will appear on the November contractual practice statements for any difference in deductions that are due for the period from 1 October 2022.
Practices must not submit a Salary Change form or revised 2022/23 Estimate of GP and non-GP provider NHS pensionable profits/pay until after the new contribution rates have been applied to PCSE Online.